Stress Urinary Incontinence is a common condition, affecting an estimated 30% of women worldwide. The condition can have a significant impact on daily life affecting activities, relationships and emotional well-being. Two thirds of these women suffering from SUI are undiagnosed.
A recent survey commissioned by Contura showed that around 9 out of 10 women living with SUI are likely to simply “put up with” the condition, rather than seeking treatment and advice, despite any negative effects on their quality of life, relationships or ability to exercise.
So, with an increasing number of celebrities and influencers breaking the taboo around the topic, it is more important than ever to openly discuss and understand which treatment options are safe and effective.
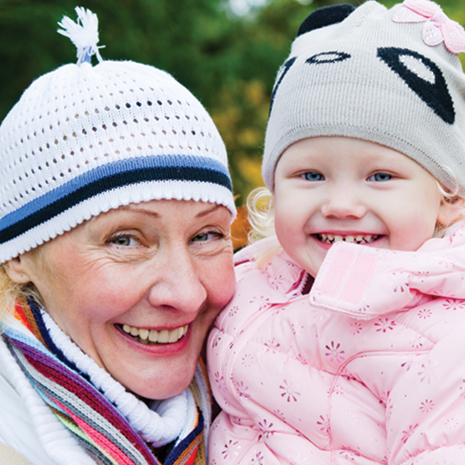
Bulking agents – Bulking agents, such as Bulkamid®, are generally lesser known than surgical approaches to treating SUI and are a minimally invasive treatment which means no cutting of the patient’s tissue or skin. They are a safe and effective treatment for stress urinary incontinence which have been used for over 10 years and is available on the NHS. Bulkamid® is a water-based gel that helps the bladder neck to close when needed to help prevent bladder leaks and has an 80% success rate when used as a first line treatment. Many of patients have been shocked by how quickly they are able to return to their normal routines after minimally invasive treatments, such as bladder bulking, and have no more leaks when partaking in exercise, sneezing or even using a trampoline with their kids.
Laser treatments – such as, the 3D-Vjuve CO2 laser and Femilift, which deliver superficial energy into vaginal skin and creates tiny white ablated dots of damaged tissue on the mucosal tissue inside the vaginal canal. The resulting heating response stimulates new collagen production improving the thickness of the vaginal lining. There is a lack of evidence that these treatments work for women suffering from SUI and a concern about the long-term safety of using lasers. These treatments are most likely to be found within private clinics.
Medical devices – If your pelvic floor muscles are weak, an inserted vaginal device may help to prevent leaks. Examples are tampons, over-the-counter pessaries and custom fitted pessaries. These devices typically press against the wall of the vagina and the urethra. The pressure helps reposition and support the urethra, leading to fewer leaks with minimal risk.
Electrical stimulation – Electrical stimulation may give patients better control over the muscles in their bladder. A small probe will be inserted into the vagina and an electrical current will run through the probe, which helps strengthen the pelvic floor muscles while exercising. Patients may find the electrical stimulation difficult or unpleasant to use, but it may be beneficial if unable to complete pelvic floor muscle contractions without it.
Whether you are a celebrity, a new mum or have just “had enough” of putting up with incontinence then speak with you GP who will be able to advise you on the best treatment pathway, for you.
For more information please visit www.bulkamid.com